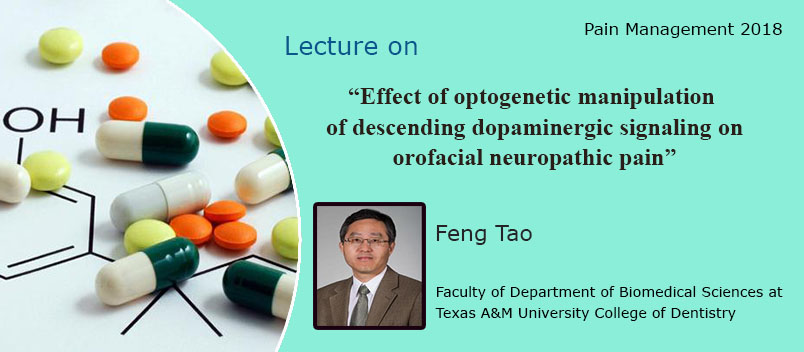
Pain Management 2019
About Conference
EuroSciCon invites all the participants i.e., Researchers, Professors, scientific communities, delegates, students, business professionals and executives from all over the world to attend “6th Edition of International Conference on Pain Management” during March 26-28, 2018 at Vienna, Austria which includes prompt Keynote presentations, Oral talks (Speaker forum and Young research forum), Poster presentations, Workshops and Exhibitions.
Pain Management 2018 is a global overview the Theme: “Unique Pioneering Research, strategies and approaches in Pain Management” which brings together professionals particularly interested in the Pain Management research work and discussions about new scientific discoveries have brought about some significant advances in the understanding of why differing approaches to the management of chronic pain are needed. There is growing evidence for the application of ultrasonography, radiofrequency ablation and neuromodulation in chronic pain management for both diagnostic and treatment applications. Techniques such as epigenetics and the use of risk stratification tools will enable personalised medicine. The quality of clinical research and lessons learned from opioid addiction have enabled the clinician to better advise their patients on the best treatments for them. This meeting showcases some of these advances placing them firmly in clinical practice.
This three day conference should enable the attendee to pick up the best in what pain management has to offer as well as highlight future directions.
Goals:
1. Growing role of diagnostic imaging modalities in management of chronic pain
2. Advances in neuromodulation techniques for chronic pain treatment
3. New understanding of psychological factors helps explain chronic pain and how it leads to powerful interventions
4. A Taster session on Pain-Specific Mindfulness interventions for chronic pain
5. Merging role of epigenetic mechanisms for chronic pain
6. Panel discussion on opioid-induced tolerance and physical dependence
Target Audience for Pain Management 2018:
Programs are of interest not only to Pain Science Professionals/Experts, but to Pharmacologist, Orthopaedist, Rheumatologist, Rheumatologist Researchers, Pharmacists, Physiotherapist, Neurologist, Pain Management Doctors, Professors, Presidents, Oncologist, Acupuncturist, Anesthesiologist-Pain Specialist, Medical Doctors, Drug Developers, Rehabilitation Doctors, Students From academe within the Study Of Pain Management And Pain Medicine.
WHO SHOULD ATTEND ?
From Private & Public hospitals and research institutes:
Designations in the hospitals and universities:
Designation of Professors in hospitals: Anaesthetics & Pain Management Consultant, Clinical Pain Psychologist, Senior Physiotherapists, Medical Pain Specialists Pain Management Nurses and departments would be Pain Management, Anaesthetics, Chronic pain services and Physiotherapy
Designation of Professors in Universities: Pain Medicine Professors, Assistant Professors, Principle Scientists, Researchers, Senior lecturers and departments would be Anaesthetics and Faculty of Pain Medicine
About Sessions
Track 1: Introduction to pain management
Pain Management can be simple or complex, depending on the cause of the pain. An example of pain that is typically less complex would be nerve root irritation from a herniated disc with pain radiating down the leg. This condition can often be alleviated with an epidural steroid injection and physical therapy. Sometimes, however, the pain does not go away. This can require a wide variety of skills and techniques to treat the pain.
There are many sources of pain. One way of dividing these sources of pain is to divide them into two groups, nociceptive pain and neuropathic pain. How pain is treated depends in large part upon what type of pain it is.
Nociceptive pain: Examples of nociceptive pain are a cut or a broken bone. Tissue damage or injury initiates signals that are transferred through peripheral nerves to the brain via the spinal cord. Pain signals are modulated throughout the pathways. This is how we become aware that something is hurting.
Neuropathic pain: Neuropathic pain is pain caused by damage or disease that affects the nervous system. Sometimes there is no obvious source of pain, and this pain can occur spontaneously. Classic examples of this pain are shingles and diabetic peripheral neuropathy. It is pain that can occur after nerves are cut or after a stroke. Most back, leg, and arm pain is nociceptive pain. Nociceptive pain can be divided into two parts, radicular or somatic.
Radicular pain: Radicular pain is pain that stems from irritation of the nerve roots, for example, from a disc herniation. It goes down the leg or arm in the distribution of the nerve that exits from the nerve root at the spinal cord. Associated with radicular pain is radiculopathy, which is weakness, numbness, tingling or loss of reflexes in the distribution of the nerve.
Somatic pain: Somatic pain is pain limited to the back or thighs. The problem that doctors and patients face with back pain, is that after a patient goes to the doctor and has an appropriate history taken, a physical exam performed, and appropriate imaging studies (for example, X-rays, MRIs or CT scans), the doctor can only make an exact diagnosis a minority of the time. The cause of most back pain is not identified and is classifies as idiopathic. Three structures in the back which frequently cause back pain are the facet joints, the discs, and the sacroiliac joint. The facet joints are small joints in the back of the spine that provide stability and limit how far you can bend back or twist. The discs are the "shock absorbers" that are located between each of the bony building blocks (vertebrae) of the spine. The sacroiliac joint is a joint at the buttock area that serves in normal walking and helps to transfer weight from the upper body onto the legs.
Track 2: Epidemiology and Classification
Epidemiology is the study and analysis of the patterns, causes, and effects of health and disease conditions in defined populations. It is the cornerstone of public health, and shapes policy decisions and evidence-based practice by identifying risk factors for disease and targets for preventive healthcare. Epidemiologists help with study design, collection, and statistical analysis of data, amend interpretation and dissemination of results (including peer review and occasional systematic review). Epidemiology has helped develop methodology used in clinical research, public health studies, and, to a lesser extent, basic research in the biological sciences.
Major areas of epidemiological study include disease causation, transmission, outbreak investigation, disease surveillance, forensic epidemiology and screening, biomonitoring, and comparisons of treatment effects such as in clinical trials. Epidemiologists rely on other scientific disciplines like biology to better understand disease processes, statistics to make efficient use of the data and draw appropriate conclusions, social sciences to better understand proximate and distal causes, and engineering for exposure assessment.
Track 3: Current Diagnosis and Scoring Systems
Emergency physicians play an important role in early diagnosis and prompt management of the conditions. Experienced emergency physicians can detect important clinical findings and give a provisional diagnosis to a patient before transferring her to general surgery or obstetrics and gynecology departments according to their judgment. Previous studies showed that some clinical indicators were helpful to distinguish appendicitis and common obstetrics and gynecological conditions (OB-GYNc) from nonspecific abdominal pain.
To resolve the difficulty in diagnosis of acute lower abdominal pain in female patients, whose appendicitis is confounded by OB-GYNc, imaging studies had been done. Imaging investigations such as ultrasonography, computerized tomography (CT), and magnetic resonance imaging (MRI) have high accuracies in diagnosis of acute lower abdominal pain. However, the universal usage of CT may not be cost-effective in countries with limited healthcare resources. In addition, time spent for such investigations is also important for the emergency department.
Clinical diagnostic scoring, on the other hand, may be more appropriate for early diagnosis in an emergency department setting. Clinical scoring for diagnosis of appendicitis was studied for its application as a guideline used for admission and investigations. However, such clinical scoring system was not designed for diagnosis of acute lower abdominal pain from obstetrics and gynecology conditions (OB-GYNc), which are also important in young adult females.
Precise and systematic pain assessment is required to make the correct diagnosis and determine the most efficacious treatment plan for patients presenting with pain.
Track 4: New Frontiers in Neuropathic Pain
The various neuropathic pains can be difficult to treat. However, with careful diagnosis and often a combination of methods of treatments, there is an excellent chance of improving the pain and return of function.
Medications are a mainstay of treatment of neuropathic pain. In general, they work by influencing how pain information is handled by the body. Most pain information is filtered out by the central nervous system, usually at the level of the spinal cord. For example, if you are sitting in a chair, your peripheral nerves send the response to the pressure between your body and the chair to your nervous system. However, because that information serves no usual purpose, it is filtered out in the spinal cord. Many medications to treat neuropathic pain operate on this filtering process. The types of medications used for neuropathic pain include antidepressants, which influence the amount of serotonin or norepinephrine, and antiseizure medications, which act on various neurotransmitters, such as GABA and glycine.
One of the most powerful tools in treating neuropathic pain is the spinal cord stimulator, which delivers tiny amounts of electrical energy directly onto the spine. Stimulation works by interrupting inappropriate pain information being sent up to the brain. It also creates a tingling in the pain extremity, which masks pain.
Track 5: Anesthesia as Pain Treatment
In the practice of medicine (especially surgery) and dentistry, anesthesia is a temporary induced state with one or more of analgesia (relief from or prevention of pain), paralysis (muscle relaxation), amnesia (loss of memory), and unconsciousness. A patient under the effects of anesthetic drugs is referred to as being anesthetized. Anesthesia is freedom from pain. Each year, millions of people in the United States undergo some form of medical treatment requiring anesthesia. Anesthesia, in the hands of qualified professionals like Certified Registered Nurse Anesthetists (CRNAs), is a safe and effective means of alleviating pain during nearly every type of medical procedure. Anesthesia care is not confined to surgery alone. The process also refers to activities that take place both before and after an anesthetic is given. In the majority of cases, anesthesia is administered by a CRNA. CRNAs work with your surgeon, dentist or podiatrist, and may work with an anesthesiologist (physician anesthetist). CRNAs are advanced practice registered nurses with specialized graduate-level education in anesthesiology. For more than 150 years, nurse anesthetists have been administering anesthesia in all types of surgical cases, using all anesthetic techniques and practicing in every setting in which anesthesia is administered. Anesthesia enables the painless performance of medical procedures that would cause severe or intolerable pain to an un-anesthetized patient.
Track 6: Current Therapy in Pain Management
To prepare for any chronic pain coping technique, it is important to learn how to use focus and deep breathing to relax the body. Pain control techniques mainly involved Altered focus. This is a favorite technique for demonstrating how powerfully the mind can alter sensations in the body. Focus your attention on any specific non-painful part of the body and alter pain sensation in that part of the body. Dissociation As the name implies, this chronic pain technique involves mentally separating the painful body part from the rest of the body, or imagining the body and mind as separate, with the chronic pain distant from one’s mind. Sensory splitting, this technique involves dividing the sensation into separate parts. Mental anesthesia This involves imagining an injection of numbing anesthetic (like Novocain) into the painful area, such as imagining a numbing solution being injected into your low back. Mental analgesia Building on the mental anesthesia concept, this technique involves imagining an injection of a strong pain killer, such as morphine, into the painful area. Alternatively, you can imagine your brain producing massive amount of endorphins, the natural pain relieving substance of the body, and having them flow to the painful parts of your body.
Track 7: Various Aspects of Opoids
Opioids are substances that act on opioid receptors to produce morphine-like effects. Opioids are most often used medically to relieve pain, and for their euphoric effects by people addicted to opioids.[3] Opioids include opiates, an older term that refers to such drugs derived from opium, including morphine itself. Other opioids are semi-synthetic and synthetic drugs such as hydrocodone, oxycodone and fentanyl; antagonist drugs such as naloxone and endogenous peptides such as the endorphins. The terms opiate and narcotic are sometimes encountered as synonyms for opioid. Opiate is properly limited to the natural alkaloids found in the resin of the opium poppy although some include semi-synthetic derivatives. Narcotic, derived from words meaning numbness or sleep, as an American legal term, refers to cocaine and opioids, and their source materials; it is also loosely applied to any illegal or controlled psychoactive drug. In some jurisdictions all controlled drugs are legally classified as narcotics. The term can have pejorative connotations and its use is generally discouraged where that is the case.
Opioids are a type of narcotic pain medication. They can have serious side effects if you don't use them correctly. If you need to take opioids to control your pain, here are some ways to make sure you're taking them as safely as possible. Opioid drugs work by binding to opioid receptors in the brain, spinal cord, and other areas of the body. They reduce the sending of pain messages to the brain and reduce feelings of pain. Opioids are used to treat moderate to severe pain that may not respond well to other pain medications.
Track 8: Pain Medications
Prostaglandins are a family of chemicals that are produced by the cells of the body and have several important functions. They promote inflammation that is necessary for healing, but also results in pain, and fever; support the blood clotting function of platelets; and protect the lining of the stomach from the damaging effects of acid.
Prostaglandins are produced within the body's cells by the enzyme cyclooxygenase (COX). There are two COX enzymes, COX-1 and COX-2. Both enzymes produce prostaglandins that promote inflammation, pain, and fever. However, only COX-1 produces prostaglandins that support platelets and protect the stomach. Nonsteroidal anti-inflammatory drugs (NSAIDs) block the COX enzymes and reduce prostaglandins throughout the body. As a consequence, ongoing inflammation, pain, and fever are reduced. Since the prostaglandins that protect the stomach and support platelets and blood clotting also are reduced, NSAIDs can cause ulcers in the stomach and promote bleeding. Narcotics also referred to as opioid pain relievers are used only for pain that's severe and is not helped by other forms of painkillers. When used rigorously and underneath a doctor's direct care, these medications are often effective at reducing pain. Narcotics work by binding to receptors into the brain that blocks the sensation of pain. When used rigorously and underneath a doctor's direct care, they'll be effective at reducing pain. Antidepressant medication for treatment of depression as well as other different disorders that will occur alone or together with depression, like chronic pain, sleep disorders, or anxiety disorders. Antidepressants are medication used for the treatment of major depressive disorder and different conditions, chronic pain and neuropathic pain. Anticonvulsants, or anti-seizure medications, work as adjuvant analgesics. In different words, they can treat some forms of chronic pain even if they're not designed for that purpose. whereas the most use of anti-seizure medication is preventing seizures, anticonvulsants do seem to be effective at treating certain forms of chronic pain. These include neuropathic pain, like peripheral neuropathy, and chronic headaches like migraines.
Track 9: Pharmacological Approaches for Pain
Acute and chronic pain may be conceptualized as either nociceptive or neuropathic in origin. A broad description of the predominating pain pathophysiology can usually be inferred through:
Patient description
Physical findings
Results of laboratory tests and imaging studies.
There are several pharmacological interventions that may be accustomed manage pain in arthritis. However, in choosing the acceptable approach, the practitioner must take into account to consider the efficacy. Adverse side effects, dosing frequency, patient preference, and cost in choosing medication for pain management. When a patient develops the primary signs of an inflammatory arthritis, the most priority is symptom relief, with pain being the cardinal sign of inflammation that patients most wish facilitate with. However, it has become more and more clear that for inflammatory arthropathies like RA merely treating the symptoms with non- Steroidal anti- inflammatory drugs (NSAIDs) or analgesics in adequate, because features of the disease that lead to damage to the joints, and then to disability will carry on uncheck. In addition to symptoms –relieving drugs, patients also need disease-modifying pain drugs that have been demonstrated to slow down or stop the damaging aspects of disease There are two aims in the pharmacological treatment; firstly to reduce inflammation or modulate the auto immune response and secondly to modulate the pain response. Medications is thought-about in 5 classes: simple analgesics, non-steroidal anti-inflammatory drugs (NSAIDs), Disease modifying anti-rheumatic-drugs (DMARD’S), Steroids, Biologics and other relevant Adjuvant analgesics (ex. antiepileptic and antidepressants used for pain relief).
Track 10: Non Pharmacological Approaches
Non-pharmacological approaches may contribute to effective analgesia and are often well accepted by patients. Some simple measures which are sometimes recommended (eg, hot or cold packs) have not been well studied. Complementary therapies for pain are often sought out by patients, and require evaluation for their potential role in the palliative care setting.
The role of non-pharmacological approaches to pain management is evolving, and some non-pharmacological and complementary therapies have an increasingly important contribution to make to holistic patient care alongside analgesics. There is evidence to support the use of patient education, cognitive behavioural therapy (CBT), relaxation, and music. Importantly, however, some approaches have not been shown to be of benefit, including TENS, reflexology and acupuncture. For this reason, research on non-pharmacological approaches to pain management is very important, so that patients are provided with information that ensures them the most effective options for treating their pain. It is essential that palliative care patients with anything more than mild pain who are using complementary therapies should also be treated with appropriate analgesics and adjuvants, using an evidence-based approach.
Track 11: Pain Management Specialist
To a certain extent, medical practitioners have always been specialized. Specialization was common among Roman physicians. The particular system of modern medical specialties evolved gradually during the 19th century. Informal social recognition of medical specialization evolved before the formal legal system. The particular subdivision of the practice of medicine into various specialties varies from country to country, and is somewhat arbitrary. Currently, there is no single field of medicine or health care that represents the preferred approach to pain management. Indeed, the premise of pain management is that a highly multidisciplinary approach is essential. Pain management specialists are most commonly found in the following disciplines: Physiatry (also called Physical medicine and rehabilitation), Anesthesiology, Interventional radiology, Physical therapy. Specialists in psychology, psychiatry, behavioral science, and other areas may also play an important role in a comprehensive pain management program. Selection of the most appropriate type of health professional - or team of health professionals - largely depends on the patient's symptoms and the length of time the symptoms have been present.
Track 12: Orofacial Pain Management
Orofaical pain is a general term covering any pain which is felt in the mouth, jaws and the face. Orofacial pain is a common symptom, and there are many causes. Orofacial pain has been defined as "pain localized to the region above the neck, in front of the ears and below the orbitomeatal line, as well as pain within the oral cavity, pain of dental origin and temporomandibular disorders". It is estimated that over 95% of cases of orofacial pain result from dental causes (i.e. Toothache caused by pulpitis or a dental abscess). However, some orofacial pain conditions may involve areas outside this region, e.g. temporal pain in TMD. Toothache, or odontalgia, is any pain perceived in the teeth or their supporting structures (i.e. the periodontium). Toothache is therefore a type of orofacial pain. Craniofacial pain is an overlapping topic which includes pain perceived in the head, face, and related structures, sometimes including neck pain. All other causes of orofacial pain are rare in comparison, although the full differential diagnosis is extensive.
Track 13: Pain Management through Nursing
Perianesthesia Nursing could be a nursing specialty practice area involved with providing medical care to patients undergoing or convalescent from anesthesia. Perianesthesia nursing encompasses many subspecialty observe space and represents a various range of practice environment and skill sets. Pain management nurses are typically thought-about to be perianesthesia nurses, given the cooperative nature of their work with anesthetists and also the fact that a large proportion of acute pain issues are surgery related. However, distinct pain management certifications exist through the American Society for Pain Management Nurses. The nurse’s primary commitment is to the health, welfare, comfort and safety of the patient. Self-awareness, knowledge of pain and pain assessment, and knowledge of the standard of care for pain management enhances the nurse’s ability to advocate for and assure effective pain management for each patient. When advocating for the patient, it is crucial that the nurse utilize and reference current evidence-based pain management standards and guidelines. The Role of nurse is responsible and accountable to ensure that a patient receives appropriate evidence-based nursing assessment and intervention which effectively treats the patient’s pain and meets the recognized standard of care.
Market Analysis
The global Pain Management market is worth around $30.9 billion in 2007. It is forecasted to grow at a compound annual growth rate (CAGR) of 5.63% to reach $40.6 billion by the end of the forecast period, 2012.
The pharmaceuticals segment of the pain-management market is valued at $29 billion in 2007. It will be worth $38 billion by 2012 at a CAGR of 5.6%.
In 2007, market revenue from the medical devices segment is around $1.9 billion. This segment is predicted to grow at a CAGR of 6.5% to reach $2.6 billion by the end of 2012.According to research report, "Global Pain Management Drugs Market: Analysis By Type (Opioids, NSAIDs, Anti-Migraine, Anticonvulsants), By Application, By Region, By Country: Opportunities and Forecast (2011-2021)" the global market is projected to display a robust growth with a CAGR of 4.96% during 2016- 2021, chiefly driven by large number of drugs in pipeline, rising number of chronically ill patients, new reforms and regulations in the consumption of medical cannabis.
Company profiled are Endo Pharmaceuticals, AstraZeneca, Novartis, Purdue Pharma, GSK, Tetra Bio Pharma, Allergen, Boehringer-Ingelheim and Sanofi,Pfizer
The report intends to provide cutting-edge market intelligence and help decision makers take sound investment evaluation. Besides, the report also identifies and analyses the emerging trends along with major drivers, challenges and opportunities in the global food service equipment market. Additionally, the report also highlights market entry strategies for various companies across the globe.
Market for global pain management pharmaceuticals and devices by revenue at manufacturers’ sales levels is projected to grow from $36.6 billion in 2014 to nearly $37.8 billion in 2015 and $44.3 billion in 2020, with a compound annual growth rate (CAGR) of 3.2% between 2015 and 2020.
Report Includes
1. An overview of the global market for pain management drugs, which will address acute vs. chronic pain, treatments, and issues facing healthcare workers.
2. Analyses of global market trends, with data from 2013 and 2014; estimates for 2015, and projections of CAGRs through 2020.
3. Examination of product categories, use of products, and the competitive landscape.
4. Coverage of several significant market trends, including undertreatment issues, professional issues, managed care pain issues, trends in new therapies, product pipelines, generic participation, pain research, drug delivery, and patent expirations.
5. Discussion of new regulatory requirements.
6. Comprehensive company profiles of major players in the industry.
Report Scope
This report is designed to be a helpful business tool that will provide a thorough evaluation of the markets for pain management. The geographical scope of this study is global. This study will address acute versus chronic pain, treatments and regulatory issues facing healthcare workers. Also provided is detailed information based on product categories, use of products, forecasts and competitive analyses.
The report identifies two general segments of pain management:
1. Pharmaceuticals
2. Devices.
Within the pharmaceuticals segment several sub-segments are discussed in detail, including:
1. Narcotic pain management.
2. Non-narcotic pain management.
3. Antimigraine treatments.
4. Anesthetics.
5. Other drugs (including fibromyalgia treatments).
The device segment covers several product lines and specifically targets the largest product segments including:
1. Electrotherapy stimulators.
2. Spine stimulators.
3. Other products (including electromagnetic therapies and other treatments).
4. For each market segment detailed information is provided based on product categories, product use, forecasts and competitive analyses.
Learn More
Top Pain Management Universities Worldwide:
University of Cambridge | EuroSciCon
Massachusetts Institute of Technology | University of Oxford | Stanford University | Yale University | University of California | Johns Hopkins University | Imperial College London | University of California | University of Cia Institute of Technology | University of Toronto | McGill University | Duke University | University of Melbourne | Columbia University | National University of Singapore | University of Chicago | The University of Tokyo | University of Pennsylvania | University of Michigan | Cornell University | University of Washington | University College London | Karolinska Institute | Sweden Rockefeller University | University of Edinburgh | The University of Sydney | University of London | University of British Columbia | The University of Manchester | University of Queensland | University of Wisconsin Madison | Boston University | Monash University | University of Texas | Kyoto University | The University of Auckland | Washington University | Humboldt Universität ZU Berlin | Erasmus University | Leiden University | McMaster University | University of Hong Kong| Australian National University | University of Helsinki | University of Bristol | New York University | Ruprecht Karls Universität | Aarhus University | Baylor College of Medicine | Brown University | Cardiff University | Dartmouth College | Freie Universität Berlin | Katholieke Universiteit Leuven | London School of Hygiene & Tropical Medicine | Ludwig Maximilians Universität | Lund University| Maastricht University | Mayo Medical School | National Taiwan University | Northwestern University | Osaka University | Pennsylvania State University | Purdue University | Queen Mary University | Technische Universität | The University of Adelaide | The University of New South Wales | The University of Sheffield | The University of Western Australia | Trinity College Dublin | Tufts University | Université Catholique de Louvain | Université de Montréal | University of Aberdeen | University of Alberta | University of Amsterdam | University of Bath | University of California | University of Copenhagen
Europe Pain Management Universities:
University of Cambridge | Massachusetts Institute of Technology | University of Oxford | Stanford University | Yale University | University of California | Johns Hopkins University | Imperial College London | University of California | University of Cia Institute of Technology | University of Toronto | McGill University | EuroSciCon | Duke University | University of Melbourne | Columbia University | National University of Singapore | University of Chicago | The University of Tokyo | University of Pennsylvania | University of Michigan | Cornell University | University of Washington | University College London | Karolinska Institute | Sweden Rockefeller University | University of Edinburgh | The University of Sydney | University of London | University of British Columbia | The University of Manchester | University of Queensland | University of Wisconsin Madison | Boston University | Monash University | University of Texas | Kyoto University | The University of Auckland | Washington University | Humboldt Universität ZU Berlin | Erasmus University | Leiden University | McMaster University | University of Hong Kong| Australian National University | University of Helsinki | University of Bristol | New York University | Ruprecht Karls Universität | Aarhus University | Baylor College of Medicine | Brown University | Cardiff University | Dartmouth College | Freie Universität Berlin | Katholieke Universiteit Leuven | London School of Hygiene & Tropical Medicine | Ludwig Maximilians Universität | Lund University| Maastricht University | Mayo Medical School | National Taiwan University | Northwestern University |
Euroscicon Ltd with immense pleasure invites all the contributors across the globe to the 2nd International conference on Food Security and Sustainability (Food Security 2017) during June 26-27, 2017 at San Diego, USA which includes prompt keynote presentations, Oral talks, Poster presentations and Exhibitions.
Euroscicon Ltd organizes 1000+ scientific events inclusive of 600+ Conferences, 500+ Workshops and 200+ Symposiums on various topics of Science & Technology across the globe with support from 1000 more scientific societies and Publishes 500+ Open Access journals which contains over 50000 eminent personalities, reputed scientists as editorial board members. Food security is often defined in terms of food availability, food access and food utilization. Global agriculture currently produces ample calories and nutrients to provide the entire world's people healthy and productive lives". However, food is not distributed equally to regions, countries, households and individuals. Improved access to food-through increased agricultural productivity and incomes-is essential to meet the food needs of the world's growing population. Successful food security and poverty-oriented programmes not only assist poor rural populations to produce more and diversified products but to produce a surplus that can be marketed and thereby generate income for the purposes of improving quality of life through improved diet and nutrition, investment in productive activity, and as collateral for credit to purchase inputs and/or other supplies to enhance agricultural or non-agricultural enterprise. Agricultural economists have maintained that greater concentration on small farmers leads to faster growth rates of both aggregate economic output and employment .Other analysts argue that production-focused service delivery directed solely at the poor as producers in isolated areas will yield low and probably diminishing returns. San Diego is a major city in California, on the coast of the Pacific Ocean in Southern California. San Diego is the eighth-largest city in the United States and second-largest in California With an estimated population of 1,394,928 as of July 1, 2015, San Diego is the birthplace of California and is known for its mild year-round climate, natural deep-water harbour, extensive beaches, long association with the United States Navy and recent emergence as a healthcare and biotechnology development center. The city is the seat of San Diego County and is the economic center of the region. Join us at Global Food Security conference for “Producing sustainable thoughts to bolster the future”. This event has been designed to address scientists, scholars, and different societies supporting food security, Industries and other related scientific communities with different levels of awareness, expertise and proactive solutions to create global impact in this field. Moreover, it will help industrialists to incorporate sustainability into every aspect of Agricultural Industries business model. The Food Security conference will influence industries to maximize their yield and profit through the application of strategic techniques. Additionally, it will reveal the best techniques to promote sustainable agricultural development and achieve a hunger free world by 2050.
We look forward to an exciting scientific event in the beautiful city of San Diego, USA.Market analysis